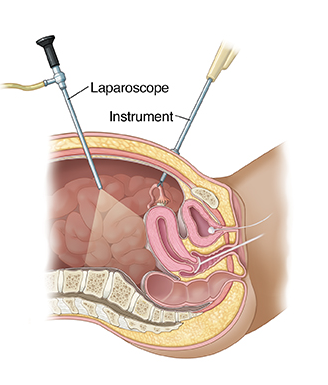
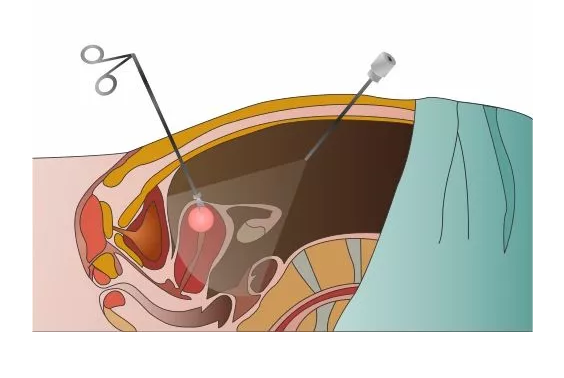
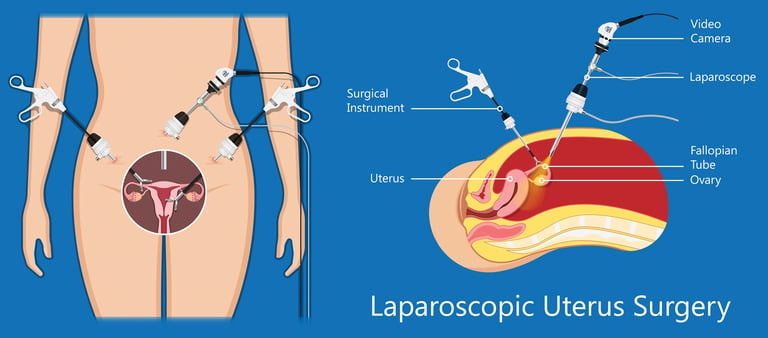
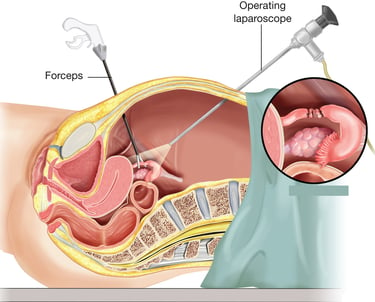
Laparoscopic surgery is a minimally invasive approach that allows the surgeon to make a surgery without making a large incision. A thin, lighted tube with a camera on the end, known as a laparoscope, is inserted into the abdomen through a small incision. The surgery is performed using surgical instruments which are inserted through 2-3 additional small incisions. The camera sends images of the inside of the body to a TV monitor in the operating room, allowing the surgeon to see and operate on the pelvic organs without having to use a long incision.
During the last 50 years, laparoscopy has evolved from a limited gynecologic surgical procedure used only for diagnosis to a major surgical tool used for many gynecologic and non-gynecologic indications. Today, laparoscopy is one of the most common surgical procedures performed in many parts of the world as an alternative to open surgery.
The advantages of laparoscopy compared to open surgery include:
Significantly less pain level after surgery.
Lower risk of complications such as infections and pulmonary embolisms after surgery.
Shorter duration of hospitalization after surgery. The length of hospitalization varies according to the type of surgery, but in the vast majority of cases, the patient stays in the hospital for one day only.
Faster return to the daily routine. A return to full activity is usually expected after about 10-14 days.
Cosmetic advantage. The incisions in laparoscopy are so small that it is sometimes difficult to notice them after a few months.
Laparoscopic surgeries are performed under general anesthesia.
There are two types of laparoscopy:
Diagnostic laparoscopy is an investigative operation and is usually undertaken to investigate the possible reasons for abdominal/pelvic pain and infertility.
Operative laparoscopy may be used to:
Treat endometriosis or pelvic inflammatory disease
Remove an ectopic pregnancy
Remove an ovarian cyst/ovary and fallopian tube or take a biopsy
Perform a hysterectomy (removal of the womb)
The preparation for the surgery included:
Basic blood and urine tests 2-3 weeks before surgery.
Chest X-ray and ECG (if needed) 2-3 weeks before surgery.
Wash the belly with soap and water the evening before surgery.
Fasting 6-8 hours before surgery.
Arrive at the hospital the evening before or early in the morning before surgery.
Meet the surgeon, anesthesiologist, and the nurse at the entrance to the operating room.
After the procedure, the patient stays in the post-operative room where the close follow-up after vital signs is performed, and pain medications are provided. After 2 hours the patient is transferred to the department and usually discharged 24-48 hours later.
Important to note that minimally invasive surgery does not mean minimal surgical experience needed to perform laparoscopy. The surgeon should be familiar with special surgical stuff and have significant experience in accurate and careful hand movements to perform the procedure safely. This experience I purchased during my 10 years of practice in Israel, Canada, and France.
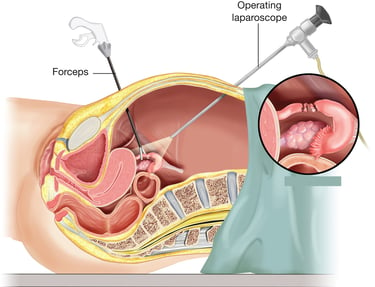
Hysteroscopy is a procedure that allows a surgeon to diagnose and treat the pathology of the uterine cavity.
A hysteroscope is a thin, lighted tube that a surgeon inserts through the vagina to examine the cervix and the inside of the uterus. For better visualization, we use a sterile fluid or gas to extend the uterine cavity. During operative hysteroscopy, the surgeon uses a thin device to remove abnormalities.
Hysteroscopy is primarily used to identify and treat conditions that cause abnormal uterine bleeding, heavy menstrual bleeding, irregular spotting between periods, and bleeding after menopause.
Hysteroscopy is used to diagnose and correct the following uterine conditions:
Polyps and fibroids. Hysteroscopy is used to find and remove these uterine structural abnormalities. The surgical removal of a polyp is called a hysteroscopic polypectomy. Surgical removal of a fibroid is called a hysteroscopic myomectomy.
Adhesions (also known as Asherman's syndrome). Uterine adhesions are bands of scar tissue that can form in the uterus and may lead to changes in menstrual flow and cause infertility. Hysteroscopy can help the doctor locate and remove the adhesions.
Septums. Hysteroscopy can help determine whether there is a uterine septum, a malformation (defect) of the uterus that’s present from birth.
Hysteroscopy may also be used to:
Diagnose the cause of repeated miscarriages or fertility problems.
Locate an intrauterine device (IUD).
Diagnose and remove placental tissue after birth
Usually, we recommend scheduling the hysteroscopy during the first week after the bleeding stops. This timing will allow the best view of the inside of the uterus. The procedure can take place at any time if the patient has gone through menopause.
Hysteroscopy can be performed:
Without anesthesia (office hysteroscopy, see and treat procedure) in case of a diagnostic procedure or relatively small pathology. In this case, the patient feels only a small discomfort.
Under anesthesia, when a large polyp/fibroid (usually over 3 cm in diameter) or a significant amount of adhesions are detected. Even in this case, the patient is usually discharged from the hospital on the same day of the procedure.
Hysteroscopy is a type of minimally invasive procedure. However, it does not mean that minimal surgical experience is needed to perform it. The surgeon should be familiar with special surgical devices and have significant experience in accurate and careful hand movements to perform the procedure safely. This experience I purchased during my 10 years of practice in Israel, Canada, and France.


An ovarian cystectomy is a procedure to remove ovarian cysts. An ovarian cyst is a sac filled with fluid or semisolid material that forms on or within one or both of the ovaries. There are different types of ovarian cysts, most of which are painless and harmless (benign). Usually, ovarian cysts don’t cause symptoms. The patient likely won’t know she has one unless the specialist finds one during a routine pelvic exam or imaging procedure. Rarely, ovarian cysts can cause complications.
Functional cysts represent the most common type of ovarian cyst and aren’t disease-related. Functional cysts generally shrink over time, usually within 60 days, without specific treatment.
Abnormal cysts
Cystadenomas. These cysts form on the surface of the ovary. They can be filled with thin and watery fluid or thicker and mucous-like.
Dermoid cysts (mature teratomas). Dermoid cysts consist of cells that make up all types of tissue in the human body, ranging from skin, hair, teeth, and even brain tissue.
Endometriomas. These cysts are filled with endometrial tissue, the same tissue that bleeds each month during the menstrual period.
Ovarian cancer. Unlike the conditions above, ovarian cancer cysts (tumors) are solid masses of cancer cells.
Signs and symptoms
Pelvic pain or a dull ache in your back. Extreme pain, nausea, and vomiting may be the signs of ovarian torsion which prevents blood flow to the ovary.
A feeling of fullness (bloating) located in the lower belly that may feel more pronounced on one side of the body.
Pain during intercourse (dyspareunia).
Painful periods.
Hormone-related problems include obesity, increased growth of body hair, and infertility.
Diagnosis
We usually use the following tests to diagnose an ovarian cyst:
Pelvic exam
Ultrasound can detect cysts on the ovaries, including their location and whether they’re primarily fluid or solid.
Computer tomography (CT) is usually done if the malignancy is suspected to determine the spread of the tumor.
Magnetic resonance imaging (MRI) is used for endometriomas and endometriosis-related lesions.
Blood tests that can indicate the risk of a non-benign finding (tumor markers such as CA 125).
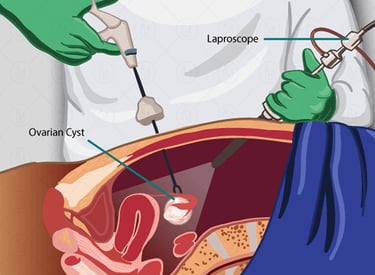
Laparoscopy is a minimally invasive surgical procedure performed under general anesthesia. We perform laparoscopy in the selected cases of persistent or abnormal cysts. The advantage of laparoscopy is that we can treat the cyst at the same time.
Treatment
Functional ovarian cysts usually go away without treatment. However, in cases of persistent or complex cysts, ovarian cystectomy can be considered. In most cases, we perform this procedure using a minimally invasive laparoscopic approach. During this procedure, we insert a small camera through a small incision in the abdomen. We rigorously revise all the organs of the abdominal and pelvic cavity including reproductive organs. The ovarian cyst can be removed through tiny incisions.
In cases when ovarian cystectomy may damage the healthy ovarian tissue we consider alternative treatment options during the laparoscopy:
Cyst ablation is when we drain the cyst fluid and burn the cyst capsule. We may perform this procedure using a special type of laser (argon or carbon dioxide) which burns the cyst superficially without damaging the ovarian tissue.
Sclerotherapy is when we fill the cyst with the sclerosing agents leading to the obliteration of the cyst.
One of the main limitations of the surgical treatment of ovarian cysts is possible damage to the healthy ovarian tissue that may cause a decrease in fertility. To avoid this the surgeon must combine deep knowledge in the field of reproduction and have high surgical skills using different surgical techniques for maximal ovarian tissue preservation.
According to the localization, endometriosis is classified as gynecological, gastrointestinal (mostly bowel), urinary tract, and distally localized which may involve the diaphragm, lungs, abdominal wall, and other organs.
Endometriosis which affects only a superficial layer of the abdominal or pelvic cavity is called peritoneal endometriosis. When endometriosis affects deeper tissues we usually call it deep infiltrating endometriosis (DIE). The endometriosis which affects the ovaries contributing to the cyst formation is called endometrioma. But here is a trick, there is no correlation between the the grade of disease and the severity of the symptoms. The patient with peritoneal endometriosis can suffer not less than the patient with DIE, and vice versa.
Endometriosis is a chronic, autoimmune, and hormone-dependent condition. The treatment is based on those characteristics and includes hormonal treatment, pain medications, nutritional changes, physiotherapy, and alternative options like acupuncture.
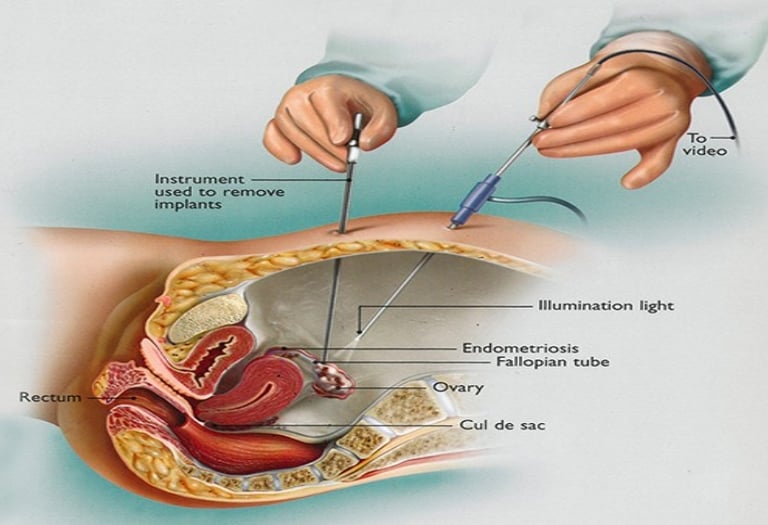
In cases when the conservative treatment is not helpful or when the patient cannot be hormonally treated (medical contraindications, hyper-sensitivity to the hormones, pregnancy desire) the specialist may consider surgical treatment. The surgery is mainly performed using the minimally invasive (laparoscopic) approach with 5-10 mm incisions on the abdominal wall.
The surgery may include the adhesions separation, superficial and/or deep endometriosis resection, ovarian cyst removal, the biopsy of the tissue suspected of endometriosis, and other modalities.
Since pelvic endometriosis nodule may involve several nearby organs (uterus, ovary, uterine tube, bladder, bowel) the surgeon's experience in the surgical treatment of endometriosis and preservation of fertility are of paramount significance.
The uterine (fallopian) tubes are the pathway for the egg to reach the uterus when conception occurs. Uterine tubes are located on the top and either side of the uterus, almost like a set of horns.
A salpingectomy is a surgical procedure where one or both of the fallopian tubes are removed. This procedure is performed to treat certain conditions of the fallopian tubes:
hydrosalpinx (the blockage of a tube caused by a fluid buildup and dilation of the tube at its end).
developing ectopic pregnancy.
as a preventative measure for women at higher risk of developing ovarian cancer.
This procedure is usually performed using a minimally invasive laparoscopic approach under general anesthesia with small incisions on the abdominal wall.


Uterine myomas (fibroids) are a common type of benign tumor of uterine muscle. About 80% of all women have uterine fibroids. The exact cause is unknown, but we know that estrogen and progesterone play a role.
Not all fibroids cause symptoms, but when they do, symptoms can include:
increased abdominal distention (enlargement).
heavy menstrual bleeding.
back pain.
frequent urination.
constipation.
pain during intercourse (dyspareunia).
There are different types of uterine fibroids depending on where they’re located and how they attach. The location of the fibroid usually explains the clinical signs it causes. Specific types of uterine fibroids include:
Intramural fibroids. These fibroids are embedded into the muscular wall of your uterus. They’re the most common type.
Submucosal fibroids. These fibroids grow under the inner lining of your uterus. This type of fibroid is usually responsible for heavy menstrual bleeding or bleeding between the menstruations causing anemia.
Subserosal fibroids. This type of fibroid grows under the lining of the outer surface of your uterus. They can become quite large and grow into the pelvis causing back pain, frequent urination, and constipation due to their pressure on the adjusted organs.
Pedunculated fibroids. These fibroids attach to the uterus with a stalk or stem. They are often described as mushroom-like because they have a stalk and then a wider top.
Fibroids can grow as a single nodule or in a cluster. Clusters of fibroids can range in size from 1 millimeter to more than 20 centimeters (8 inches) in diameter or even larger.
The uterine myomas can be diagnosed using:
Pelvic exam.
Ultrasonography.
Magnetic resonance imaging (MRI).
Computed tomography (CT) scan.
Hysterosalpingography(HSG).
Sonohysterography is when the provider places a small catheter in your vagina and then injects saline into your uterus. This extra fluid helps to create a clearer image of your uterus than you would see during a standard ultrasound.
Small fibroids often don’t need treatment, but larger fibroids can be treated with medications or surgery.
The surgical treatment is considered in cases of significant symptomatic fibroids when the conservative treatment has failed. The type of procedure that may work best will depend on where the fibroids are located, and how big they are. The types of myomectomy (fibroid removal) procedures can include:
Hysteroscopy is when we insert a small camera into the uterus through the vagina. Then we use small manipulators to cut away and remove the fibroids.
Laparoscopy. In this procedure, we use a few small incisions in the abdomen to remove the fibroids. We use a special device (morcellator) to cut and remove the fibroids from the abdominal belly to avoid the widening of incisions.
Laparotomy. In extreme cases when the fibroids are huge and very symptomatic we make one larger incision in your abdomen and remove the fibroids through this one cut.
If the woman does not plan future pregnancy, there are additional surgical options that may be considered according to the size and location of fibroids:
Hysterectomy (uterus removal) is a definitive treatment of fibroids. By removing the uterus completely, the fibroids can’t come back and the symptoms should go away. If the ovaries are left in place, the patient will not go into menopause after a hysterectomy, but will not have the menstrual bleeding. This procedure might be recommended if the patient is experiencing very heavy bleeding from the fibroids or fibroids are large. Minimally invasive hysterectomies include laparoscopic or robotic methods.
Uterine fibroid embolization is when an interventional radiologist puts a small catheter in the uterine artery and injects small particles, which then block the flow of blood from the artery to the fibroids. Loss of blood flow shrinks the fibroids and improves the symptoms.
Since uterine fibroid treatment may include a few modalities and approaches, the deep knowledge of the reproduction field and extensive surgical skills of the surgeon are critically essential.
A hysterectomy is a surgical procedure that removes the uterus. It’s the second most common surgery performed among women (after Cesarean section). Depending on the reason for the surgery, a hysterectomy may involve removing surrounding organs and tissues, such as the fallopian tubes and ovaries. Hysterectomy leaving ovaries will not cause the signs of menopause.
The main indications for hysterectomy include:
Abnormal or heavy vaginal bleeding that isn’t managed by other treatment methods.
Severe pain with menses and suspected adenomyosis that isn’t managed by other treatment methods.
Uterine fibroids cause pain and abnormal uterine bleeding.
Uterine prolapse (uterus that has “dropped” into the vaginal canal due to weakened support muscles) leads to urinary incontinence or difficulty with bowel movements.
Cervical or uterine cancer or abnormalities that may lead to cancer for cancer prevention.
Conditions with the lining of the uterus, like hyperplasia or recurrent uterine polyps.
The main types of hysterectomy include:
Total hysterectomy: removing the uterus and cervix, but leaving the ovaries.
Supracervical (subtotal) hysterectomy: removing just the upper part of the uterus while leaving the cervix.
Total hysterectomy with bilateral salpingo-oophorectomy: removing the uterus, cervix, fallopian tubes (salpingectomy), and ovaries (oophorectomy). If the patient has not experienced menopause, removing the ovaries will probably start menopausal symptoms.
Radical hysterectomy with bilateral salpingo-oophorectomy: the removal of the uterus, cervix, fallopian tubes, ovaries, the upper portion of the vagina, and some surrounding tissue and lymph nodes. This type of hysterectomy is performed when cancer is diagnosed.
There are several different surgical approaches to perform a hysterectomy:
Vaginal hysterectomy is when the uterus is removed through an incision at the top of your vagina. There isn’t an external incision.
Laparoscopic hysterectomy is when a laparoscope (a thin tube with a video camera on the end) is inserted in the lower abdomen through a small incision in the belly button. Surgical tools are inserted through several other small incisions. The uterus can be removed in small pieces through the incisions in the abdomen or the vagina without the need to extend the small incisions on the abdominal wall.
Robotic-assisted laparoscopic hysterectomy is when the surgeon performs the procedure with the help of a robotic machine. Small, thin surgical tools are inserted through three to five incisions around the belly button. Robotic arms and instruments are controlled by the surgeon.
Abdominal hysterectomy is when the uterus is removed through a 9-10 cm incision in the abdomen. This approach is most commonly used when cancer is suspected or when the uterus is significantly enlarged.
Whatever approach is chosen the high level of surgeon's experience in the gynecological and general surgery is of paramount significance.
Ovaries are reproductive glands that release hormones to control the menstrual cycle and promote bone and heart health. Ovaries also contain and help grow eggs leading to pregnancy.
A surgeon may remove one or both ovaries for several reasons, including:
Preventative surgery for people at a higher risk of breast and ovarian cancer (BRCA gene mutation carriers).
Ovarian cancer.
Certain cases of ovarian torsion.
Certain cases of an infection of the ovary or the area around it, also known as a pelvic inflammatory disease (PID)or a tubo-ovarian abscess (TOA).
Certain cases of large endometrioma (cystic lesions that stem from the disease process of endometriosis).
There are several different types of oophorectomies:
Unilateral oophorectomy: removing one ovary (one side).
Bilateral oophorectomy: removing both ovaries (both sides).
Salpingo-oophorectomy: removing one ovary and one uterine tube.
Bilateral salpingo-oophorectomy: removing both uterine tubes and ovaries.
There are various ways a surgeon can remove an ovary. Each procedure carries its own risk and recovery time.
Laparoscopic approach is considered a minimally invasive approach. The surgeon uses a small camera to look inside the abdomen. The surgeon makes other small 1-2 cm incisions on your skin to allow for the removal of your ovary. Laparoscopic surgery has a smaller risk of infection and the patient usually recovers faster. In some cases, the surgeon may perform the surgery with the assistance of a robotic arm moving the instruments (while the surgeon guides them).
Vaginal approach is also considered a minimally invasive approach, with a smaller risk of infection and faster recovery.
Laparotomy (open surgery). In some cases, the surgeon decides that a larger incision is needed to complete the surgery. This incision is known as a laparotomy, and it involves cutting into the abdomen. Laparotomies, or bigger incisions, usually have a longer recovery time and higher risk of complications, although these are still low.
Most people resume their normal routines 2-4 weeks after surgery. Removing both ovaries will cause menopause to begin immediately. Hormone replacement therapy can help patients deal with symptoms caused by menopause.
Whatever approach is chosen the high level of surgeon's experience in the gynecological and general surgery is of paramount significance.
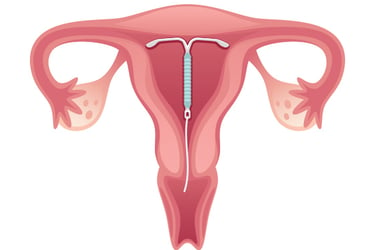
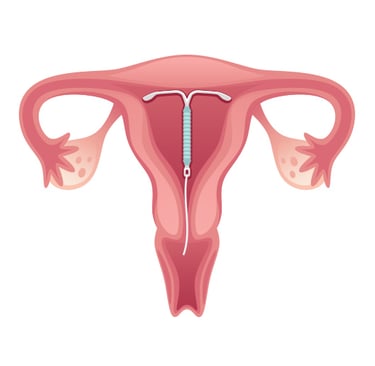
An intrauterine device (IUD) is a type of birth control a healthcare provider inserts into the uterus. IUDs are the most commonly used type of long-acting reversible contraception. Once an IUD is inserted, the patient does not have to worry about birth control until it’s time to replace it (3-5 years, depending on the brand). If the patient decides to become pregnant, the provider can remove the IUD.
There are two kinds of IUDs:
Copper IUD which has a thin copper wire that coils around the stem part. This IUD heightens the inflammatory response, causing the uterine lining (endometrium) to become inflamed. Even if sperm were to fertilize an egg, the uterine lining would make it difficult for a fertilized egg (embryo) to implant there and develop.
Hormonal (levonorgestrel) IUD which contains the progestin hormone levonorgestrel, which flows through the stem. Progestins are a synthetic version of progesterone, a hormone that occurs naturally in a female's body. This IUD releases small amounts of the progestin hormone levonorgestrel over time. Levonorgestrel thickens the cervical mucus, making it harder for sperm to swim to the uterine tubes. It also thins the uterus lining and partially suppresses the ability to release an egg during the menstrual cycle.
The advantages of using an IUD include:
99% success rate.
Prevention of having to locate contraceptives before having intercourse.
IUD can be removed if the patient decides to become pregnant or switch birth control methods.
Prevention from getting pregnant for years without any ongoing maintenance on the patient's part.
Spare the worry of having missed a birth control pill, forgotten to get a birth control shot, etc.
Hormonal IUD reduces heavy menstrual bleeding.
Hormonal IUD relieves menstrual cramps and pain from endometriosis.
IUDs are considered both safe and effective. Complications - while rare - may include:
Expulsion when IUD may slip out of the uterus. When this happens, it usually occurs during the period, within the first few months after it’s been inserted.
Perforation is when the uterine wall can be pierced during insertion.
High-risk pregnancy. The chances of becoming pregnant with an IUD are slim. On the off chance that the patient does become pregnant, the extrauterine pregnancy should be excluded.
Infection. Bacteria can enter the body when the IUD is inserted, causing an infection. Infections are most likely to occur within the first 20 days of insertion.
What happens before, during, and after an IUD insertion:
The patient may need to take a pregnancy test or get tested for STIs beforehand.
The provider may consider pain management before the procedure.
The provider may consider performing an ultrasound test to evaluate the uterine cavity before the procedure.
The provider will use a speculum to widen the vagina and clean the cervix during IUD insertion to lower the risk of infection. The patient may feel mild to intense cramping during the IUD insertion.
The provider may perform another ultrasound test just after the procedure and request an additional ultrasound test 2-3 weeks later to confirm the right IUD position in the uterine cavity.
Contraindications for IUD application include:
Pregnancy.
Active or high risk for sexually transmitted infection (STI).
Cervical, ovary, or uterine cancer.
Unexplained vaginal bleeding.
Copper IUDs should not be used in case of copper allergy or Wilson disease, a genetic condition that causes copper to build up in the body.
Hormonal IUDs should not be used in case of severe liver disease or breast cancer.
Fertility preservation saves and protects the embryos, eggs, sperm, and reproductive tissues. This helps make it possible to have a child sometime in the future.
Hereby we will speak about fertility preservation in women which may be done for two reasons:
Elective preservation is when someone wishes to delay having children for personal reasons
Medically indicated preservation is when fertility may be compromised due to health conditions or diseases which include:
Certain types of chemo- and radiotherapy potentially harmful to fertility.
Certain auto-immune diseases.
Before the surgical treatment of ovarian cysts including large endometriomas.
Fertility preservation methods for benign conditions in women include:
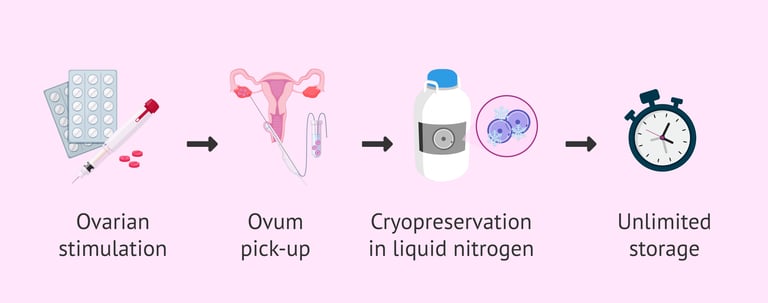
Egg freezing. During this process, the patient receives hormonal medications to stimulate egg production in the ovaries. When at least 3 follicles achieve a 17-18 mm diameter, we provide the last injection for the last stage of oocyte maturation and trigger the ovulation. Thirty-six hours later we perform the procedure called ovum pick-up (OPU) which is done through the vagina with ultrasound guidance to retrieve the oocytes from the ovaries. Then, eggs are frozen and stored.
Embryo freezing. Similar to egg freezing, this involves the collection of eggs from the ovaries. Then the eggs are fertilized with the partner’s sperm or donated sperm, creating embryos. This procedure is called in vitro fertilization (IVF). Then the embryos are frozen and can be implanted in the uterus after the thawing.
Ovarian tissue freezing is performed If the patient is already receiving cancer treatment or there is no time to wait the two to six weeks needed to receive hormone treatment for egg or embryo cryopreservation. Instead, we may consider removing and cryopreserving some ovarian tissue. This procedure is performed by laparoscopy under general anesthesia when a small camera is introduced inside the abdomen and other small 1-2 cm incisions are done on the skin to allow for the removal of ovarian tissue. After the cancer treatment, we may reimplant the thawed tissue using another laparoscopy. If the tissue regains function, the patient may be able to become pregnant spontaneously or via IVF.

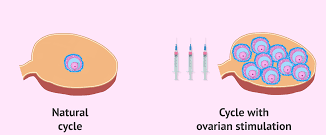
When we are speaking about ovarian stimulation we mean the hormonal drug administration to stimulate the ovary and induce or to boost the follicle growth process.
We usually distinguish two main tactics to stimulate the ovaries:
Controlled ovarian stimulation (COS) to trigger the growth of 1-3 dominant follicles following timed intercourse or intrauterine sperm insemination. The doses of administered medications (oral or injectable) are relatively low to avoid the development of an excessive number of follicles preventing the patient from multifetal pregnancy and ovarian hyperstimulation syndrome.
Controlled ovarian hyperstimulation (COH) is a part of the IVF process which involves the administration of higher doses of injectable hormones to stimulate over 3 follicles. When at least 3 follicles achieve a 17-18 mm diameter, we provide the injection for the last stage of oocyte maturation and trigger the ovulation. Thirty-six hours later we perform the procedure called ovum pick-up (OPU) which is done through the vagina with ultrasound guidance to retrieve the oocytes from the ovaries. Then the eggs are fertilized with the partner’s sperm or donor sperm, creating embryos. This procedure is called in vitro fertilization (IVF). Three to five days later one or few embryos are transferred to the uterus, and others can be frozen and saved for further transfers.
The main (although relatively rare) complication of ovarian stimulation is ovarian hyperstimulation syndrome (OHSS) which typically occurs in people who receive fertility treatments that stimulate their ovaries to produce a large number of eggs. This is more common with injectable medications that stimulate the ovaries. New protocols and strategies have made this condition less common, although severe cases still occur from time to time.
Symptoms of mild to moderate OHSS include:
Abdominal pain.
Bloating.
Slight weight gain.
Nausea.
In more severe cases of OHSS, symptoms may include:
Excessive weight gain.
Severe nausea and vomiting.
Severe abdominal swelling.
Difficulty breathing.
Blood clots.
Decreased urination.
Severe abdominal pain.
The treatment for OHSS varies depending on how severe the condition is. Treatment aims to manage symptoms and avoid complications. Mild cases tend to go away within a week or two. However, if the patient gets pregnant during that cycle, the symptoms could last much longer.
For mild to moderate cases of OHSS, treatment usually involves:
Avoiding vigorous physical activity.
Drinking electrolyte-rich fluid.
Using acetaminophen to relieve symptoms.
Weight control.
Monitoring for any severe symptoms.
Severe cases of OHSS often require hospitalization. Treatment of severe OHSS may include:
Receiving intravenous (directly into the vein) fluids.
Undergoing paracentesis (a procedure to remove fluid from the belly).
Taking medicines to ease symptoms or reduce activity in the ovaries.
A blood thinner to help decrease the risk of a blood clot.
Sometimes hospitalization is required for supportive care and close monitoring until symptoms improve. Both COS and COH should be done under the supervision of specialists with experience in the field of reproduction.
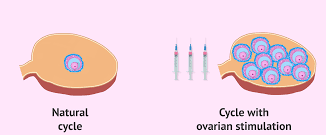
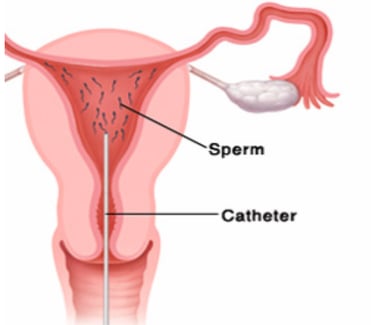
Intrauterine insemination (IUI), a type of artificial insemination, is a fertility treatment where sperm is placed directly into a woman’s uterus.
During a natural conception, sperm has to travel from the vagina through the cervix, into the uterus, and to the uterine tubes. This is where the sperm and egg meet and fertilization occurs. Only 5% of the sperm are able to travel from the vagina to the uterus.
With IUI, the sperm is collected, washed, and concentrated so that only high-quality sperm remain. This sperm is placed directly into the uterus with a catheter (thin tube), putting it closer to your fallopian tubes. There is no need for anesthesia for this procedure. IUI makes it easier for the sperm to reach an egg because it cuts down on the time and distance it has to travel. This increases the chance of becoming pregnant.
We often perform IUI synchronized with controlled ovarian stimulation. IUIs can be performed with the partner’s sperm or with donor sperm.
Intrauterine insemination (IUI) may be used when these conditions are present:
Low sperm count or other sperm impairments. IUI can help to overcome these problems because only high-quality sperm cells are selected and used for IUI.
Cervical mucus problems or other problems with the cervix. The cervix separates the vagina and uterus from each other. The mucus produced by the cervix helps sperm travel from the vagina through the uterus. Thick mucus can make it hard for sperm to swim. With IUI, sperm bypasses the cervix and goes directly to the uterus.
Using donor sperm. IUI is used when people use sperm from a person who isn’t the birth parent’s partner. This is called donor insemination (DI). DI is done when one partner has no sperm or when the sperm quality is so low that the sperm can’t be used. Single women or same-sex female couples who wish to conceive can also use donor sperm.
Ejaculation or erection dysfunction. IUI can be used when one partner can’t get or sustain an erection or isn’t able to ejaculate.
Semen hypersensitivity. In rare cases, women have a high sensitivity to their partner’s semen. It can cause burning, swelling, and redness in the vagina. IUI can be effective because the proteins causing the allergy are removed during sperm washing.
Unexplained infertility. This is when we do not reveal an exact reason for infertility.
In vitro fertilization (IVF) is a type of infertility treatment where eggs are combined with sperm outside of the body in laboratory conditions.
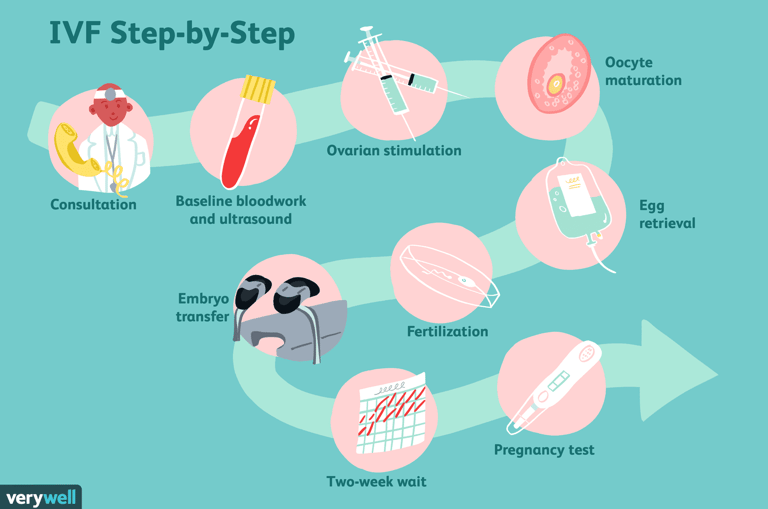
IVF is only one step of the infertility treatment using artificial reproduction technology:
Preparation for treatment including the revision of the infertility reason and previous infertility treatment.
Performing some routine tests before IVF (blood test, cervical PAP test, ovarian reserve test, sperm test).
Controlled ovarian hyperstimulation using both stimulating and suppressing injectable medications to induce and control the development of a few ovarian follicles containing oocytes. This usually takes 12 to 14 days.
Ovum pick-up procedure to retrieve the oocytes from the ovaries which is usually done under short general anesthesia with ultrasound guidance. The procedure usually takes 20-30 minutes and the patient will leave the hospital 2-3 hours later.
Partner sperm (after masturbation or testicle biopsy) or donor sperm preparation.
In vitro fertilization (IVF) itself when the embryologist places the oocytes and sperm cells in a dish nutrients or performers the injection of sperm into each mature egg (intracytoplasmic sperm injection, or ICSI).
Embryo development which is carefully monitored every day.
Embryo transfer three to five days after the egg retrieval with ultrasound guidance. The patient will take some oral and/or vaginal hormonal medications to maintain the pregnancy development after embryo transfer.
Freezing the surplus embryos and eggs for embryo transfer in the future.
Pregnancy test 12-14 days after embryo transfer.
The specialist may consider postponing the transfer of embryos in case of endometriosis or ovarian hyperstimulation syndrome. In this case, the embryologist will freeze all embryos after the egg retrieval and fertilization. The patient will recover from the ovarian hyperstimulation and the embryos will be thawed and transferred into the uterus one month later. This is called the "Freeze all" protocol. The success rate of the tactic is similar to fresh embryo transfer.
If the patient has spare frozen embryos, she will not need to undergo ovarian stimulation again with the injectable hormones, but only to prepare the uterine lining for embryo transfer usually providing oral or vaginal medications, or using the natural hormonal cycle.